Industry Report
Study Oversight Implications of ICH GCP E6(R3) for Outsourced Sponsors
November 2025 | Version 3
Rapid advancements in drug development are increasing clinical trial complexity and costs, necessitating an adaptable and rigorous approach to trial oversight. The ICH GCP E6(R3) guideline took effect on 23 July, 2025, addressing this shifting clinical trial landscape while building on the established principles of Good Clinical Practice (GCP) outlined in ICH E6(R2).
While the core principles of GCP remain the cornerstone of the guideline, R3 introduces a new era of proactive, risk-based approaches with heightened emphasis on data quality. The emphasis on a more holistic approach requires fully or heavily outsourced sponsors in Europe to look closely at how they can adapt and thrive under the new guidelines.
This is especially important against the backdrop of increased hybrid inspections, where inspectors request direct access to clinical systems used for sponsor oversight throughout the trial. Fully outsourced sponsors may face a greater risk of inspection findings than their insourced peers, given that they have less control over external operations. While sponsors can delegate duties to CROs, they cannot delegate overall trial responsibility.
This whitepaper presents the findings of a cross-industry working group comprising sponsors and CROs. The goal is to explore the intricacies of ICH E6(R3), analyze its implications for outsourced sponsors, and provide valuable insights to ensure a smooth transition to the new guidance.
1. Key changes for fully and heavily outsourced sponsors
The transition from ICH E6(R2) to R3 will significantly impact sponsors that outsource their clinical trials, with key changes including:
Essential records vs. documents
R3 introduces a critical shift that emphasizes capturing and maintaining "essential records" rather than solely focusing on "essential documents." Essential records encompass a broader range of information beyond formal documents, including electronic data, communication logs, and other process-related materials.
This expanded definition requires a more comprehensive approach to operational data management and oversight in outsourced settings. Sponsors must ensure their contracts with service providers clearly define ownership, access, and retention procedures for all essential records throughout the trial lifecycle. The term “service providers” encompasses all partners delegated or contracted by the sponsor to perform duties and tasks under the sponsor’s responsibility, including CROs.
Sponsors will also need their own clinical oversight systems, such as an eTMF and CTMS, to document and demonstrate continuous oversight processes. This includes study documentation and operational data. Sponsors need to prove this continuous oversight throughout the trial, not only when it ends, and ensure records and audit trails are readily accessible during an inspection.
Direct access to essential records
R3 mandates that sponsors and investigators have direct access to all essential records, regardless of format or location. This ensures transparency and facilitates real-time monitoring and oversight throughout the trial.
Focus beyond the outcome
R3 requires more than the final documented outcome of a process. Sponsors are expected to capture their rationale and decision-making processes throughout the trial. In an outsourced context, this means sponsors must record both their decision-making and that of their CROs throughout the course of the trial. Sponsors should establish mechanisms to review and understand the rationale behind critical decisions made by the CRO, ensuring alignment with trial objectives and risk management plans.
Sponsors remain ultimately responsible for any critical decision delegated to a CRO. Therefore, maintaining documented evidence of adequate, ongoing oversight is essential. Under R3, effective oversight must be continuous, not retroactive.
Proactive quality by design
While R2 advocated for a risk-based approach to quality management, R3 pushes for a more proactive "quality-by-design" philosophy. This enhanced approach integrates quality considerations into the trial's design, execution of the study, and oversight. Sponsors working with CROs will need to ensure their partnerships foster a collaborative environment where quality is prioritized from the outset.
Although sponsors have historically relied solely on eTMF documentation, current regulatory guidance mandates a more comprehensive approach to trial oversight. Achieving inspection-readiness now demands more than a final, retrospective quality review. Instead, sponsors must embed robust quality processes from the outset, ensuring continuous oversight and proactive management throughout the trial lifecycle.
Joint planning sessions that integrate quality risk management into trial design, ongoing communication, and study oversight will be crucial for success under R3.
Sponsors also need to understand and document CRO quality processes built into CRO systems. This ensures QC processes are evidenced in their audit trails and can be transferred to the sponsor in real-time for oversight.
Strengthened risk-based sponsor oversight
R3 places a greater responsibility on sponsors to ensure quality throughout the outsourced trial. The guideline mandates clear documentation and oversight of all delegated activities. Sponsors will need to strengthen their oversight capabilities to effectively monitor CRO performance and ensure compliance with R3 requirements. This may involve investing in qualified sponsor personnel such as sponsor oversight managers or site engagement managers, establishing robust risk management plans, implementing rigorous vendor management practices, and investing in technology to execute risk management plans.
In parallel, sponsors must also invest in direct sponsor-site relationships to build trust, accelerate issue resolution, and maintain visibility. Although CROs can facilitate operational execution, they may not maintain staffing continuity or fully support investigator engagement. This is especially relevant for sponsors operating in Europe’s highly diverse small- and medium-sized biopharma landscape, where relationships and reputation can influence investigator retention and patient enrollment.
Increased role-based training and training oversight requirements
R3 brings a new focus on training programs, requiring that sponsors ensure their personnel – as well as personnel at sites, CROs, and other functional service providers – are adequately trained on GCP guidelines, trial protocols, and their trial roles.
R3 also places additional onus on investigators to provide training oversight. Regulatory authorities recognize that an increasing number of team members beyond investigators are involved in trials. Investigators were previously responsible for their site’s oversight, but now they must also provide appropriate training documentation. This includes training for specific tasks outside the usual standard of care.
Inspection findings often stem from two root causes: inadequate training or insufficient oversight. From a compliance perspective, undocumented training is considered not to have happened. Even if training did occur, this lack of evidence jeopardizes the site's reputation, the sponsor's compliance, and the integrity of the collected data. Providing sites with structured electronic tools mitigates this risk, allowing for real-time, remote monitoring and documentation.
Sponsors can support sites with their internal processes, invest in solutions to streamline how investigators assign and track training in validated systems, and ensure real-time oversight. Embracing these principles will empower outsourced sponsors to navigate the clinical trial landscape with confidence and compliance.
Emphasis on “fit-for-purpose” technology systems
To meet regulatory standards, clinical trials must utilize validated, "fit-for-purpose" computerized systems. These platforms must ensure data integrity, facilitate sponsor oversight, and maintain a complete audit trail. Crucially, system implementation and validation must be proportionate to the trial protocol, participant risk, and data criticality.
2. Barriers to effective study oversight: process, technology, and resource challenges
Outsourced study oversight requires complex orchestration between sponsors and CROs to ensure a safe, effective, and compliant trial. But, both process and technology barriers can hamper effective oversight, creating inefficiency and risk. Some of the most common challenges impacting sponsors and CROs include:
2.1. Process challenges
Inability to analyze issues or trends in real-time
Monthly review meetings between CROs and sponsors to discuss study progress and flag issues are a common practice. CROs need significant time and resources to prepare for these meetings, and data often lags four to six weeks behind. As a result, sponsors do not have a real-time view of trial progress or potential issues, undermining their ability to make timely, data-driven decisions.
Additionally, issues that surface during review meetings are not easily reportable. Issues are often defined and documented individually in the eTMF for a given trial. This process does not allow sponsors to analyze trends across multiple studies or CROs, making it difficult to identify common issues or take broad corrective action.
Delayed feedback is a primary cause of control mechanism failures. By the time a deviation is identified, the operational situation may have already changed, rendering the data obsolete. This forces a response to an outdated problem, which often triggers a cycle of new deviations leading to overcorrection or inaction.
Insufficient documentation of decision-making and issue management
Regulators expect sponsors to make risk-based, proportionate decisions — and to document those decisions appropriately throughout the trial. However, sponsors often struggle with documentation when key decisions are scattered across emails, slide decks, or SharePoint folders. When a documented process is in place, decisions can be captured with structured methods that ensure team-wide transparency, rather than being hidden in a limited email thread.
Limited visibility into investigator relationships
When CROs are the primary point of contact for investigators and sites, sponsors might lose visibility into which individuals are conducting the trial. Sponsors that do not invest in building rapport with investigators risk losing real-time communication and early detection of challenges such as staff turnover.
Inadequate evidence of oversight
Following oversight processes and procedures alone is not sufficient — sponsors must be able to show regulators proof of study oversight (e.g. the records). Even when sponsors have a clear oversight plan, the distributed nature of the work across sponsors and CROs makes it very difficult to clearly document actions and the resulting mitigations.
2.2. Technology challenges
eTMF is helpful, but not sufficient
eTMF stores essential study documents, including the oversight plan, to help inspectors evaluate the conduct of a study and the quality of data. However, with R3’s emphasis on essential records, eTMF is no longer sufficient to fully satisfy regulatory requirements.
An eTMF is a powerful document management tool, but it falls short in demonstrating active sponsor oversight, like decisions and issue resolution. The TMF is defined as the complete collection of essential trial records, regardless of their location. Consequently, essential documents held in other systems are still considered part of the TMF and are subject to the same regulatory scrutiny.
Fragmented record-keeping systems
While eTMF provides one centralized system for study documentation, other types of records that demonstrate trial oversight are often widely distributed across various technologies. This may include spreadsheets, email, shared drives, documents, SharePoint, data lakes, and visualisation tools. These solutions do not maintain audit trails, are not fit-for-purpose, and cannot serve as inspectable as essential records.
Storing essential records outside the official TMF often compromises their metadata. From a regulatory perspective, losing metadata like an audit trail can be equivalent to losing the record itself. For a critical record, this loss threatens the trial's integrity and can alter its risk-benefit assessment. Email management is a prime example. Current practices often fail to meet regulatory standards, as many teams lack a process for storing essential emails for the 25-year post-study period that authorities require.
Cumbersome and incomplete metadata
Sponsors typically do not have full visibility into the complete library of relevant records and associated metadata, such as monitoring visit reports or issues. This is often a byproduct of fragmented and ill-suited technology.
In addition, sponsors need to migrate inspectable records generated by the CRO at the end of the study, but these migrations are cumbersome. In many cases, sponsors cannot anticipate the sheer volume of metadata from the CRO, or they may receive incomplete data.
Inspectors require direct access
R3 stipulates that inspectors must have direct access to all trial-related records, requiring sponsors to make their live clinical oversight systems available for inspection. Providing read-only access to a static set of documents is no longer sufficient.
Consequently, relying on paper-based methods presents considerable logistical challenges. For example, collating and indexing thousands of paper records for an inspection can be an inefficient and resource-intensive process under these modern standards.
2.3. Resource challenges
Shifting operating models require new approaches
Although European sponsors have historically outsourced both systems and processes to CROs, they are increasingly bringing key systems in-house to improve oversight and control. This either involves bringing processes in-house or requiring CROs to work in the sponsor’s systems, moving from full-service outsourcing (FSO) to functional service provisioning (FSP).
R3 offers an opportunity for sponsors to evaluate and refresh their operating models. Although such changes require analysis and change management, sponsors can expect to increase trial efficiencies and reduce costs.
Legacy staffing models may be insufficient
Sponsors are also finding that legacy staffing models may be insufficient to provide adequate oversight throughout the trial. There is a growing trend to employ sponsor oversight managers or site engagement managers to conduct co-monitoring and oversight visits to complement CRO resources and processes.
3. How to adapt oversight processes for efficiency, quality, and compliance
Although eTMF has introduced standardized approaches to essential documentation management across sponsors, no common framework exists for operational oversight. A lack of defined standards makes it difficult for sponsors to ascertain the true inspection-readiness of their essential records. In this section, we will share best practices curated from the working group's collective experiences.
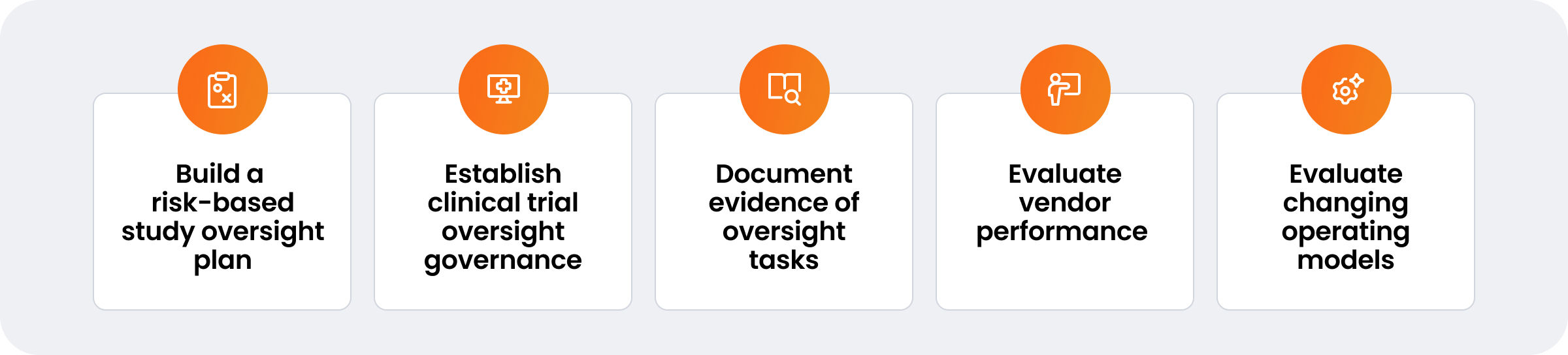
3.1. Build and document a risk-based study oversight plan up front and revise it as necessary
Effective sponsor oversight begins with a well-structured plan that delineates which essential records require review, the frequency of reviews, and the employees responsible for conducting them. The following steps are critical in constructing a comprehensive oversight plan:
Step #1: Define essential data and review parameters
Identify the specific set of data (essential records) that requires review. Determine the frequency of these reviews and assign responsibility to qualified individuals. Emphasize both the quantity and quality of resources, ensuring the team has substantial oversight experience and expertise.
Step #2: Adopt a risk-based approach
Tailor the oversight strategy based on the type of trial, its phase, and the associated risks. This ensures that higher-risk areas and sites receive appropriate attention. As applicable, co-define acceptable ranges, previously referred to as quality tolerance limits (QTLs), for in-scope activities with relevant CROs or sites.
Step #3: Implement adaptive planning processes
Define processes to continuously adapt oversight planning and actions based on emerging risks.
Step #4: Ensure CROs provide essential records in real-time
Engage CROs early in the process to align on expectations and responsibilities. Determine how CROs will provide oversight data such as quality issues, protocol deviations, documents, and associated audit trails in real-time. Sponsors may choose not to work with CROs that cannot provide this information in the format they expect. During this early engagement, sponsors can also establish CRO-focused KPIs.
Step #5: Define sponsor roles for site relationship management
Some small- and medium-sized sponsors, particularly those in late-stage development or approaching commercialization, may maintain small in-field medical science liaison teams to build scientific relationships with key investigators. These individuals often have scientific or therapeutic area expertise and aim to foster long-term relationships with high-performing sites. It is essential to define how these sponsor roles integrate with CRO-led operations to avoid misalignment, ensure consistent messaging, and document relevant site interactions as essential records.
Step #6: Establish KPIs for decision-making and resulting actions
Develop KPIs that will help identify oversight issues. These may include metrics for study progress, deviations, monitoring visit report (MVR) timeliness, quality issues, and time taken to resolve issues. Then, document actions to resolve identified issues.
Step #7: Prepare a contingency plan
Ensure that a contingency plan is in place to address unexpected issues that may arise during the trial.
3.2. Establish study oversight governance
Governance is a crucial component of effective clinical trial oversight. It ensures that oversight issues are identified, addressed, and resolved systematically and transparently. Establishing a robust framework for governance involves regular discussions, decision-making, and documentation. The following steps outline the key elements of oversight governance:
Step #1: Form an oversight governance team
Establish an oversight governance team that goes beyond the traditional study team by incorporating members with diverse, cross-functional expertise. This might include representatives from clinical operations, data management, quality assurance, and regulatory affairs. Define clear roles and responsibilities within the governance team to ensure that each member understands their duties and contributions to the oversight process.
Step #2: Create and recruit for dedicated sponsor oversight roles
To complement the cross-functional oversight governance team, consider allocating the responsibility of study-level oversight to an oversight manager or a study/ trial operations manager (SOM/ TOM).
Step #3: Schedule regular oversight governance meetings
Weekly meetings ensure continuous monitoring and timely identification of issues. They also allow for quick adjustments and proactive management of potential problems. A well-structured agenda should include a review of study progress, deviations, quality issues, and other relevant KPIs. Ensure that all team members have access to the agenda and relevant documents prior to the meeting.
Step #4: Identify and document trends
Use continuous data reviews and oversight tasks to identify patterns that may indicate systemic problems or recurring challenges in the trial. Regular trend analysis helps identify the root causes of recurring problems and develop preventive measures.
Step #5: Update oversight risk assessments
Update oversight risk assessments regularly based on identified trends and new information. This ensures that the oversight plan remains adaptive and responsive to emerging risks.
Step #6: Document risk appropriate and risk proportionate decision-making
Effective oversight requires thorough documentation of all governance meeting decisions — including those involving vendors — within validated systems. The goal is to demonstrate that these decisions are proportionate to the level of risk. This documentation must capture the rationale for each decision, the data reviewed, and the actions taken to reach the desired outcome.
Proportionality does not require that actions must scale linearly with risk. Rather, it involves reducing risks to acceptable levels through effective and justifiable measures. To be proportionate, a control's benefits should justify its cost and complexity. A measure that fails to achieve this outcome may not be an effective use of resources.
Step #7: Engage CROs on issues
Communicate identified oversight issues with CROs promptly, and document the communication in a validated system rather than email. This ensures that CROs are aware of the issues and can take appropriate actions to resolve them. Continuously monitor CROs’ progress in resolving oversight issues. Evaluate the effectiveness of the resolution actions and ensure that they meet predefined quality and timeliness standards.
Ensure that there is documented evidence that oversight governance processes have taken place. This includes minutes of oversight meetings, decision logs, communication records with CROs, and evidence of issue resolution. It should be easily accessible and auditable in a validated system to demonstrate compliance with regulatory requirements and internal standards.
3.3. Create and document evidence of oversight workflows, tasks and study data reviews
Continuous data review and oversight tasks are pivotal to maintaining trial integrity. The key steps include:
Step #1: Distribute oversight tasks
Assign oversight and data review tasks to specific study team members, ensuring clarity in roles and responsibilities.
Step #2: Review CROs’ study operational data
Review CROs’ study operational data regularly and in near real-time, with a focus on records that present the highest risk to the trial.
Step #3: Review site data
Review — or ensure CROs review — site data regularly. This includes real-time tracking of site receipt and acknowledgement of safety letters, essential documents, and training. It also includes periodic reviews of distributed documents with reporting on site compliance and adherence.
Step #4: Document site interactions
Implement solutions to retain institutional memory. Digitize sponsor/ CRO-site interactions, such as escalations tracked per site, and document continuous oversight throughout the trial.
Step #5: Document task completion
Maintain documentation as evidence of oversight task completion. This includes tracking deviations and maintaining communication logs.
Step #6: Record oversight issues
Document any oversight issues that arise, noting the specific data reviewed to inform decision-making.
Step #7: Track evidence of oversight records in validated systems
Establish a clear record to maintain data integrity, demonstrate regulatory compliance, create audit trails, and improve transparency. This can also help identify cross-study trends or areas of improvement.
3.4. Evaluate vendor performance
Effective vendor evaluation ensures vendors meet required performance standards and contribute positively to the success of the clinical trials they are involved in. A dedicated vendor evaluation team plays a crucial role in this process, ensuring thorough and consistent assessments. Below is a detailed approach to evaluating vendor performance:
Step #1: Define a vendor evaluation team
Assemble a vendor evaluation team that includes representatives from clinical operations, procurement, quality assurance, regulatory affairs, and data management. This ensures a comprehensive evaluation from multiple perspectives. Clearly define the roles and responsibilities of each team member in the evaluation process. Train team members to effectively evaluate vendor performance, emphasizing the importance of both the quantity and quality of resources, including their oversight experience and expertise. The vendor evaluation team can be an agile team or a dedicated function, sometimes referred to as an outsourcing management (OM) function. OM functions are typically a combination of procurement, PMO, and clinical operations team representatives.
Step #2: Define performance KPIs
Establish clear and measurable KPIs for vendor performance. These KPIs should reflect critical aspects of the vendor's responsibilities, such as data quality, adherence to timelines, regulatory compliance, responsiveness, and cost management.
Step #3: Review vendor performance continuously
Conduct vendor performance reviews regularly. The frequency of these reviews should be based on the complexity and volume of trials the vendor is involved in. Use predefined KPIs to assess vendor performance. Based on findings from performance reviews, implement CAPAs as necessary. Maintain thorough documentation of all discussions and decisions made during performance review meetings. This includes specific performance issues, agreed-upon actions, and timelines for improvement.
Step #4: Establish a loop for vendor engagement and improvement
Establish a continuous feedback loop with vendors. Provide constructive feedback based on performance reviews and work collaboratively on improvement plans. If there are performance issues, develop and implement performance improvement plans in collaboration with vendors. These plans should outline specific steps, responsibilities, and timelines for addressing issues.
Step #5: Assess vendor performance
Conduct retrospective evaluations of how CROs perform, including ways of working, proposed governance charters, and KPIs/ acceptable ranges to understand what forward-looking mitigation measures should be put in place.
With this study oversight framework in place, the next section will focus on best practices sponsors can adopt to improve the quality and efficiency of the process.
3.5. Evaluate your changing operating models with CROs
As an increasing number of European sponsors consider bringing systems and processes in-house to increase oversight and ensure direct access to data in real-time, they must adapt their operating models. The following steps provide a framework for evaluating an existing operating model and navigating the change to a new model:
Step #1: Conduct an activity split assessment
Transitioning from a fully outsourced operating model to bring key systems and/ or processes in-house requires detailed analysis. For instance, sponsors often start by bringing systems like EDC in-house, while keeping the associated services fully outsourced. The activity split between sponsors and CROs will differ per function and depend on a sponsor’s appetite for risk, cost, and efficiency needs. Sponsors can also assess whether activities should be executed or just managed internally. The activity split assessment represents the starting point to developing a coherent and conducive hybrid operating model.
Step #2: Redesign your operating model
Transitions of this scale need to be underpinned by a custom operating model that spans all relevant functions and serves as a go-to reference for post-transition operations. Sponsors should assess the critical challenges per function and then understand if their current technology stack can support their target model. Moreover, they must understand the relevant in-system roles, responsibilities, ownership, and activities required to support each scenario. The operating model should ultimately serve as a guide on ways of working, communication lines, data strategy, and governance mechanisms.
Step #3: Implement change management and business processes
The shift to bring systems and/ or processes in-house also entails a significant degree of change management for the sponsor’s end-users. For some end-users, business-as-usual activities will change and potentially be split with external stakeholders/ vendors. Sponsors must manage the change they will experience to ensure a smooth transition and high adoption rate of the new setup. Equally important is the alignment of internal business processes to the new setup (e.g., depending on what activities are shifted in-house, functional business processes need to be revamped in alignment with the new setup).
Step #4: Establish transition governance
Transition initiatives also require a broader decision-making group that can make timely decisions while also validating function-specific changes or requirements. At a minimum, governance should be defined with two governing bodies. This forum should retain final decision-making rights and represent the highest levels of authority for risks that manifest during the transition. Firstly, the executive steering group (ESG) is the overarching body of governance. It will be formed after the transformation efforts are complete and comprises cross-functional stakeholders (e.g., business, compliance, regulatory, and IT). Secondly, the transition oversight board (TOB) is an ancillary body of governance for the transition. The TOB will be formed at the early stage of transition and before the transformation efforts are complete.
4. Success factors for improved oversight quality and efficiency
Preparing for ICH E6(R3) may require a mindset shift for sponsors, who are ultimately responsible for a study's execution. Even when they can delegate duties to CROs, they cannot delegate oversight. Sponsors will need experienced personnel who can establish and execute oversight tasks and leverage clinical systems to keep essential records for inspections. This includes the following steps:
Step #1: Define study oversight
Oversight is often confused with supervising CRO performance, rather than its true purpose: overseeing GCP compliance, proactively mitigating risks to patient safety and data integrity, and responding promptly to issues. Ideally, vendor oversight should drive service excellence and mitigate risks through practices, processes, and tools designed to get full value from vendors throughout the partnership. Optimal vendor oversight should create visibility into GCP compliance, vendor contracts, relationship objectives, quality of work, and performance tracking. The goal is efficient and compliant delivery of contracted products and services, guaranteeing timely action and escalation when issues arise. Sponsors should define the scope of outsourced activities and establish clear transition points, which are crucial to ensure proper oversight and integration between outsourced and in-house activities.
Step #2: Create an oversight model focused on people, process, technology, and data
A sponsor’s internal capabilities and strategic vision may shift over time. Fully or heavily outsourced sponsors will benefit from a scalable oversight model built for the long term.
Sponsors should begin by defining when given study activities will be outsourced. Then, oversight should include cross-functional internal processes that account for global and local nuances. Change management is critical as internal sponsor teams will require support if outsourcing needs or regulations shift over time.
Sponsors should invest in the right clinical systems and infrastructure – beyond study documentation – to achieve optimal oversight. Technology enables real-time monitoring of study progress, early identification of potential issues, and efficient communication between study partners. Automation can support timely and streamlined data ingestion from multiple external and internal sources as well. By leveraging advanced analytics and automation, sponsors can make data-driven decisions, reduce operational costs, and improve oversight.
Step #3: Embed a culture of oversight
Study oversight should be embedded in the design of quality processes across the entire multi-disciplinary team. While clinical operations may lead the process, every team involved in the trial needs to be accountable and document records accordingly. This collaborative approach ensures comprehensive oversight and reduces the risk of errors or delays. While CROs can provide valuable expertise and resources, sponsors must ensure that CROs have the necessary tools, information, and support to execute the trial effectively. Strong collaboration at the outset can help avoid potential issues and ensure both parties achieve their common goals.
Step #4: Remain open to restarting and refreshing
R3 presents an opportunity for sponsors to reevaluate their operating models. Sponsors are increasingly bringing key systems in-house to address data ingestion challenges and to increase control and transparency in trial operations.
5. Embracing the evolving clinical trial and oversight landscape
More than 20 heavily outsourced sponsor and CROs headquartered in Europe contributed to the guidance in this whitepaper on the implications of ICH E6(R3). This working group will continue to share, update, and refine this whitepaper. As the guideline nears its 2025 release date, outsourced sponsors have a narrow window of opportunity to revisit their approach to study oversight. They may need to update ways of working with CROs, adopt new fit-for-purpose technologies, clearly define data flows, and manage change within their organizations to ensure compliance.
Ultimately, sponsors should recognize this new guidance as an opportunity to create a proactive, risk-based approach for study oversight and to ensure their study teams, CROs, and other collaborators execute safe, effective, and successful clinical trials.
Learn why every organization needs a validated oversight system for compliance.
